By GARRY RAYNO, InDepthNH.org
CONCORD — Instituting a new work requirement for able-bodied people on the state’s Granite Advantage Medicaid program was opposed by medical providers, advocates for the disabled, mentally ill, greater healthcare access, and substance abuse treatment and recovery Wednesday.
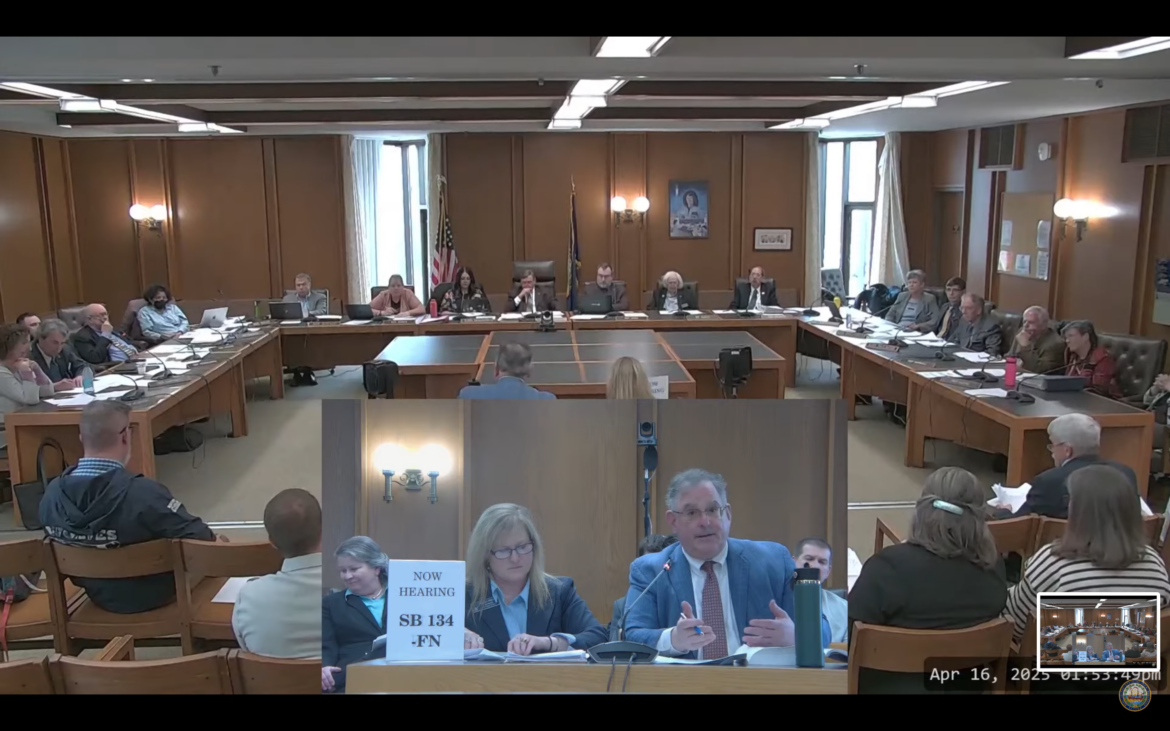
Senate Bill 134 would require the Department of Health and Human Services to seek a waiver from the Center of Medicaid Services to institute a work requirement for the Granite Advantage or Medicaid expansion program that has been in place for over a decade serving largely low-income adults.
The bill was approved by the Senate on a party line 15-8 vote and would require HHS to submit the waiver by Jan. 1.
The legislature passed a work requirement for the program about a decade ago, and the state spent $4.4 million, and was prepared to spend another $1.6 million to implement the program, but the waiver was withdrawn after a federal district court struck down the program and that decision was upheld by the circuit court of appeals.
HHS officials now estimate the program would cost about $4 million annually to implement the monthly reporting requirements still in state law and the exemptions approved a decade ago.
The prime sponsor of the bill, Sen. Harold Pearl, R-Loudon, said the requirement would help low-income families work their way out of poverty, noting the Granite Advantage program is intended to “be a bridge, not a destination.”
The state prides itself on its work ethic and the work requirement would be a good policy for the state, he said.
HHS officials told the House Health and Human Services and Elderly Affairs Committee most people are on the program for less than a year.
They also said about 65 to 66 percent of the 60,119 people on the program as of Feb. 28 work either full or part time.
The exemptions for disabilities, physical or mental health issues, single-mothers, care givers, students, etc. account for another 36 percent, using national averages, said Raymond Burke, of NH Legal Assistance. That means the bill would target a sliver of 8 percent of those on the program, he said, but the work requirement would affect everyone on the program who would have to prove monthly they are either exempt or working or volunteering.
“An exemption is not a safeguard, eligible people will be losing coverage,” Burke said. “Medicaid is health insurance and health assistance, it is not an employment program and that is why it was struck down.”
Eight percent of the 69,119 people on the Granite Advantage program is 4,810 people.
Several committee members questioned the cost of setting up a large administrative structure costing millions of dollars a year.
“Why do you want to create a large administrative structure when you are dealing with folks who may not make it to one year?” asked Rep. Janet Lucas, D-Campton.
The one person testifying in support of the bill beside the sponsor was former HHS Commissioner and current Executive Councilor John Stephen, who works as a Medicaid consultant and helped Arkansas with its waiver request to CMC for a work requirement.
Georgia is the only state to implement a work requirement, while five or six other states have applied for waivers under the Trump administration, which has indicated its willingness to support the work mandate. The Biden administration did not accept waiver requests for work requirements.
Stephen said there is nothing stopping HHS from submitting a waiver request on its own.
He noted the state led the country in 2006 when it overhauled its Temporary Assistance for Needy Families TANF program which included a work requirement when he was commissioner.
At the time about 15 or 16 percent of people on TANF were working, but after the change that went to 40 percent, he said.
“We were one of the top in the United States,” Stephen said. “We did a great job and helped move people to self independence and to help their own families.”
The unemployment rate is low in New Hampshire, he noted, so there is a need for able-bodied workers.
Stephen called the requirement a strong policy statement for the state, as other states move in this direction.
He also took issue with the cost the department estimates to stand up the program, noting much of the work was already done 10 years ago and should be a foundation.
But Henry Lipman, HHS director of Medicaid Services, said they would have to submit the waiver under the law the state currently has which requires 100 hours of work or volunteering, although other states require 80 hours, and with the exemptions in law with some changes based on what the agency has learned since that time.
A plan amendment is another option, he said, which would be less expensive, but noted the earlier law requires monthly reports that will need to be verified which is work intensive and with a 23 percent vacancy rate and a hiring freeze, it is significant additional work.
Karen Hebert, HHS director the division of economic stability, said the same staff works on multiple programs so the additional work could impact other programs if they get behind with the certifications and people are moved off the program.
Lipman noted some people go on Granite Advantage temporarily while waiting to be approved for a disability for example, and if they are moved off, they often qualify for traditional Medicaid which is a 50/50 match from the federal government and not the 90 percent federal, 10 percent state of Granite Advantage.
He said the cost projections are to pick up where they left off from the other program with a call center and outreach to those affected to ensure they do what they have to do to remain on Medicaid.
He said the last time they expected about 20,000 people to lose coverage because of the work requirement and it was about 16,000 when they halted the program and they expect a similar number if the waiver is approved.
“We are not saying do or don’t. We do have a law on the books that needs a second look,” Lipman said, noting the Granite Advantage plan does not use general fund money so there will be no cost savings to offset the $3.7 million to implement the requirement.
“There will not be any savings to be had during the (next) biennium,” he said.
Rep. Jessica LaMontagne, D-Dover, said if 65 are already working and a lot of other people qualify for exemptions maybe only about 10 percent are the target.
Yet a lot of people already working will lose coverage because of the reporting requirements, she noted.
“That is a lot of administrative expense without changing the number of people working,” LaMontagne said.
Advocates for the state’s vulnerable populations said the work requirement bill will do the people they represent great harm and would put their healthcare coverage at risk.
Krysten Evans of ABLE NH, which advocates for the disabled, said, “This bill is not just misguided, it is a direct threat to the health and safety and dignity of people with disabilities across New Hampshire.”
She said they are terrified of losing their Medicaid coverage.
“This will not increase employment, and this will not reduce poverty,” Evans said. “What it will do is punish people with disabilities for the barriers they face.”
Nancy Vaughan, government relations director for the American Heart Association, said the proposal will increase the risk of losing Medicaid, without any increase in employment, with high administrative costs and increased burdens on staff and agencies.
People’s physical and mental health challenges will lead to losing coverage, she said, because it is difficult for people and physicians to provide the verification the program will require.
“The thing you do not want to see is disruption in care if you lose coverage,” she said. “That will increase uncompensated care particularly in the rural areas and that will raise health insurance premiums for everyone.”
Kris McCracken, President and CEO of Amoskeag Health, a federally qualified health center, said Medicaid patients are a large share of the work they do.
When the work requirement was implemented the last time, she said, many of the people they serve lost their coverage, but the center is still required to provide health care to those individuals which becomes uncompensated care and the center has to absorb the costs.
The House budget has a 3 percent reduction in provider rates and federal funds are being reduced, she noted.
“In the end, are we really moving the needle,” McCracken said, “in saving funds or putting people back into the workforce.”
New Futures, National Alliance on Mental Illness, the Community Mental Health Centers, and TLC Recovery Centers all had representatives testify in opposition to the bill.
The committee did not make an immediate recommendation on the bill.
Garry Rayno may be reached at garry.rayno@yahoo.com.
Click the links below to tell your lawmakers what you think of various bills.
HOUSE
House meeting schedule for April – For schedule, click day, week or month
House Sign-in Form and Online Testimony Submission
View House Online Testimony Submissions
House Remote Sign In/Submit/View Testimony Directions (PDF)
Watch House committee meetings and sessions
SENATE
Senate meeting schedule for April For schedule, click day, week or month
Senate Remote Sign In
Senate Remote Sign In Directions (PDF)
Watch Senate committee meetings and sessions