By GARRY RAYNO, InDepthNH.org
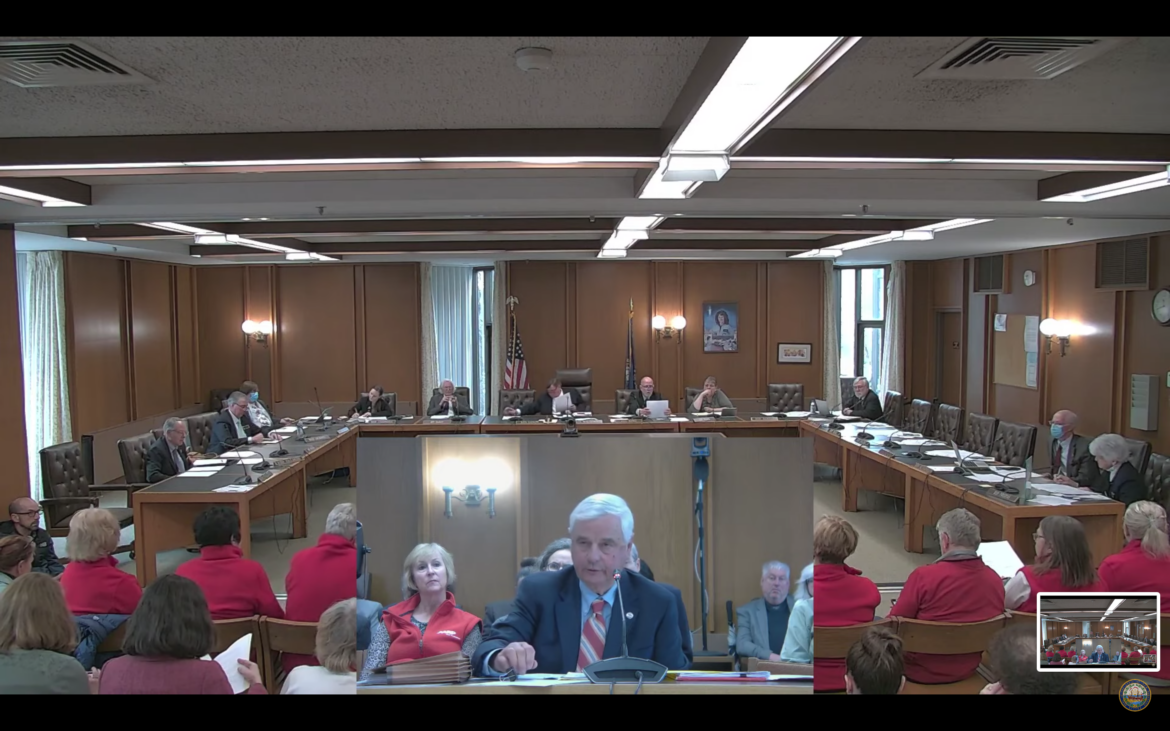
CONCORD — Advocates, health care providers, business organizations, cancer survivors, recovering addicts and patients of mental health services testified in support of a bill to reauthorize the state’s Medicaid expansion program permanently.
They also helped answer the question Senate Bill 263’s prime sponsor, Senate President Jeb Bradley, said was the only one that needed to be addressed by the House Health and Human Services and Elderly Affairs Committee.
“I hope the question you will ask that the Senate asked, ‘Has Medicaid expansion worked?’ and I believe the answer is a resounding ‘yes,’” Bradley said
During the three-hour hearing, all but one person urged the House committee to reauthorize the program and to make it permanent, as David Juvet of the Business and Industry Association said, “This is not a new program. We have 10 years of experience so it makes no sense to reauthorize it for two years and come back and reauthorize it again.”
The House Finance Committee budget plan, which the House votes on Thursday, only reauthorizes the program for two years, which Bradley and others said would cause problems with consistency for health care providers and businesses, and a permanent program will allow the state to negotiate a better financial contract with the managed care organizations that administer the Granite Advantage Health Care Program along with regular Medicare.
The lone voice in opposition to both reauthorizing the contract and making it permanent was Greg Moore of Americans For Prosperity, a Koch Foundation organization.
He noted the program has “a welfare benefit cliff” which could be a disincentive for someone to return to work.
He said the program has “an induced demand” that has added hundreds of millions of dollars to the marketplace leading to over utilization of services resulting in workforce shortages across the state.
He suggested a two-year reauthorization would allow lawmakers to quickly respond to any changes in the program.
But supporters said there are many protections built into the statutes including beginning the reauthorization process if the federal government fails to meet its requirement to cover 90 percent of the cost, or if the state needs to use general funds to cover its obligation.
And Bradley noted any member of the legislature can introduce a bill any time to change the system.
Rye physician Tom Sherman who was a House member when he was on the original commission working to establish the expansion program under the Affordable Care Act, took issue with Moore saying the program is a disincentive to work.
“This doesn’t keep people off work, it actually gets them back to work and off public assistance,” said Sherman who ran for governor last year losing to incumbent Gov. Chris Sununu. “This is the key to getting them back into the workforce to getting their dignity, their life and their economic stability back.”
He told of two of his patients who struggled with health issues until they joined the program and rebounded.
Bradley told the committee that while the program has been in place for 10 years, individuals are only on it a short time until they regain their health and can work again. Bradley and Harry Lipman, who is the state’s Medicaid director, said 70 percent of the people on Medicaid expansion do work.
The state program has a work requirement, but it has never been implemented because of a federal court decision outlawing a similar provision in another state.
Bradley touted the reduction in uncompensated care for hospitals for serving those who cannot afford to pay for the services they receive. Many people without healthcare insurance use hospital emergency rooms, which are more expensive than having a personal care physician.
He noted uncompensated care is a hidden tax on everyone with private health insurance in the state, which falls on both employers and employees.
Steve Ahnen, president and CEO of the New Hampshire Hospital Association, said his organization and the state have been partners serving the state’s most vulnerable people under the program.
“As a result of this coverage, these patients are able to receive the right care, at the right time and at the right place,” Ahnen said. “It is an important investment in the health of our state and the people we serve.”
He said the amount of uncompensated care has dropped from $173 million in 2014, the first year of the program, to $69 million in 2021.
Mark Bonta of Greenfoot America in Littleton and a member of the board of a Recovery Friendly Workplace, said he had to fire an employee who came to work under the influence of alcohol and died a few months later because he could not stop drinking.
Bonta said he later learned there are other options to get help and the people who go through that have a strength of character to beat addiction, that make them “the people I want to work for me.”
He said he had mostly success in hiring recovering addicts but like most companies there is a three-month waiting period before health benefits kick in and they need the Medicaid expansion program to see them through to keep fighting their addiction.
Doug McNutt representing the NH State Commission on Aging, said the expansion which covers those earning 138 percent of poverty level or below helps people between the ages of 56 to 64 years old. If someone in that age group loses their job, it is very hard to find another one with the same pay and benefits, and insurance coverage is very expensive, he noted.
He said about 15 percent of the people in the Medicaid expansion program are in that category. The program allows them to stay healthy while they look for another job, McNutt said.
Kris McCracken, CEO of Amoskeag Health, the largest federally qualified health center in the state, said they primarily serve those with limited incomes and resources.
She said over 50 percent of their patients are on the expansion program.
She told of a patient in his mid 50s, who was a construction worker with diabetes whose sugar levels were out of control.
But after he was on Medicaid expansion, his levels were much better, she said, and when he was asked why, he said now he could afford his medicine, to buy his test strips and do the testing.
Now he is not going to lose a limb or his eyesight, McCracken said, from the impact of a chronic disease.
“If not for Medicaid expansion, we would not be able to help them effectively manage their care,” she said.
Dylan Knowles, who runs Home Sober Living in Manchester, said he grew up impoverished and was on Medicaid as a kid.
He told the committee he was a great student and athlete, but became addicted to prescription opiates and “fell off a cliff.” Knowles said he received services he could not afford on his own through Medicaid expansion and that is why he is alive today.
“This is not speculation, this is not a guess,” Knowles said. “I know this worked really well.”
Juvet told the committee the bill is the most important bill outside of the budget for job growth and the state’s economy this session.
“This bill is important to the New Hampshire employer community,” Juvet said. “If it goes away, $1 billion over the biennium will not come into the state.”
The committee did not make an immediate recommendation on the bill, which if it initially passes the House, will go to the House Finance Committee for review before final passage.
Garry Rayno may be reached at garry.rayno@yahoo.com.