By GARRY RAYNO, InDepthNH.org
CONCORD — House and Senate negotiators reached agreement Thursday to allow the Health and Human Services Commissioner to waiver any suspension for non-compliance with the work requirement passed last year in the reauthorization of the Medicaid expansion program.
Under proposed changes, the work, school, training or community service requirement would be waived for about 20,000 participants that Health and Human Services Department officials have been unable to contact before the provision begins July 1.
The penalties for failure to meet the 100-hour a month work requirement could be loss of health coverage.
The Granite Advantage program serves about 50,000 low-income adults, many of whom work, and others are exempt.
“This bipartisan compromise protects the health care coverage for 50,000 Granite Staters,” said conference committee chair Senate Majority Leader Dan Feltes, D-Concord. “That is what Senate Bill 290 is all about. I hope Gov. Sununu signs this.”
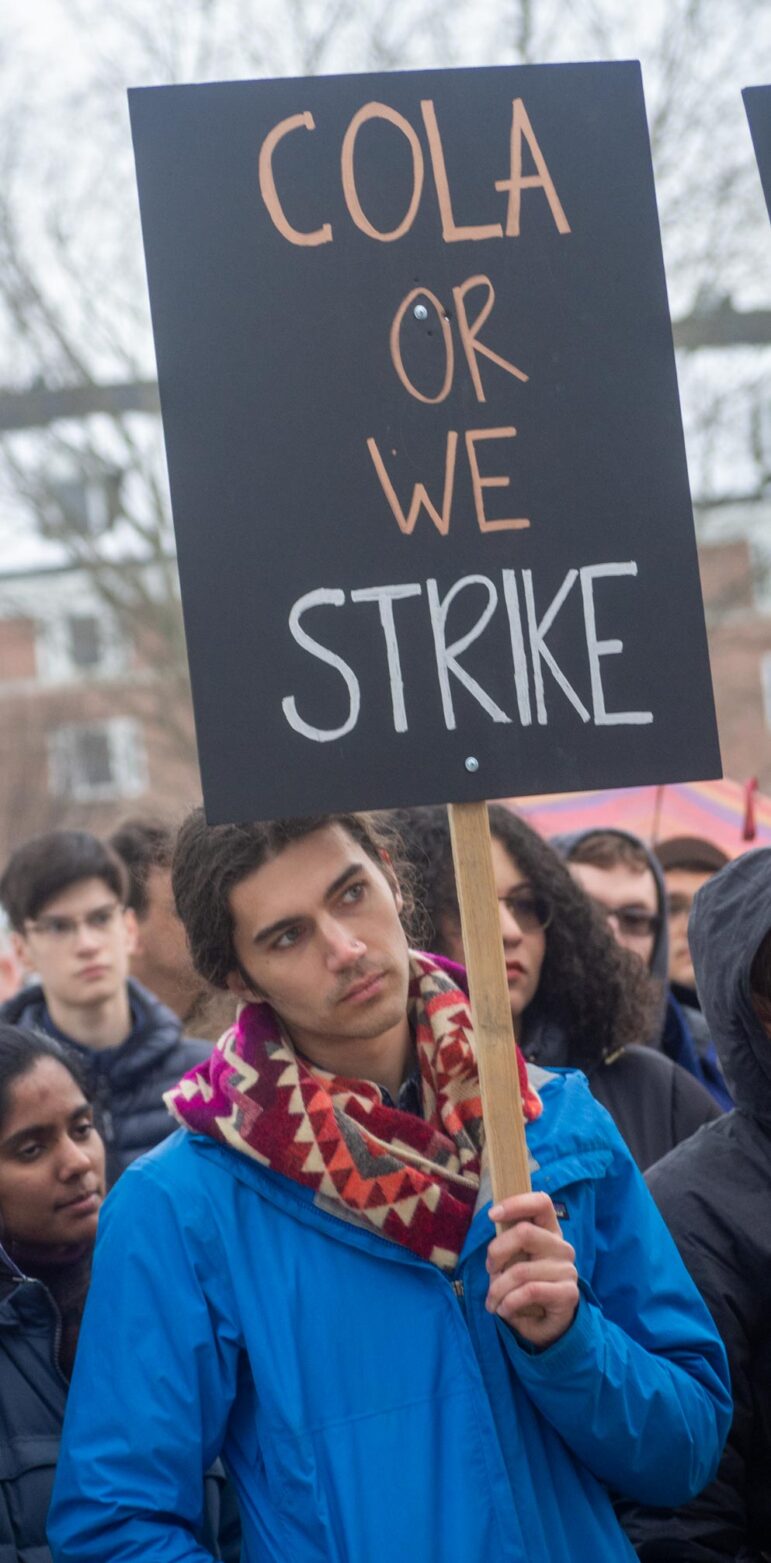
Republicans have called Democrats’ proposed changes to the work requirement a breach of last year’s agreement reauthorizing the state’s Medicaid expansion program or Granite Advantage Health Care, for five years, but Democrats said they want to ensure people on the program do not needlessly lose their health-care coverage.
Democrats passed bills that would eliminate the requirement if more than 500 people lose their coverage or uncompensated care costs rise for providers, particularly hospitals, but those triggers are not in the final agreement.
Under the agreement reached Thursday, the commissioner would be authorized to waive any suspension until July 1, 2021, by which time lawmakers hope all participants of the program could be contacted and a new legislature would have to address the issue.
Sen. Jeb Bradley, R-Wolfeboro, said Thursday Health and Human Services officials did all they could to contact the 50,000 participants, but failed to reach 20,000, which is the reason for the commissioner’s waiver. He expects the number of un-contacted people working or falling under the exemptions would reduce that number significantly.
It would be very problematic if those 20,000 participants were to lose their health coverage, Bradley said, but noted the work requirement was essential for the bipartisan support to reauthorize the program last year and will be needed in the future to continue the program.
“We can now work with (HHS) Commissioner Meyers to implement this regardless of what happens in the federal courts,” Bradley said. “This is a compromise and we’re all a little bit uncomfortable with this.”
Nationally, work
requirements are under fire and litigation is now underway.
A similar
provision to New Hampshire’s in Arkansas resulted in tens of thousands of
participants losing their health-care coverage.
The agreement reached Thursday also directs the commissioner to seek a waiver to the program’s federal approval to allow a 45-day, retroactive coverage to people qualifying for the program.
The plan would exempt parents with children 12 years old and younger and those in treatment and recovery from the state’s opioid epidemic, the lack of available work or services in a region, or no transportation.
Also, caregivers would be exempt, as would pregnant women, a person with disabilities or who is homeless, physically frail or a domestic abuse victim.
Under the Affordable Care Act, the federal government pays 90 percent of the cost of the Medicaid expansion program, while states are required to pay 10 percent.
In New Hampshire, hospitals and insurance companies pay the state’s 10 percent share.
The House and Senate will vote on the agreement June 27.
Garry Rayno may be reached at garry.rayno@yahoo.com